Treating the Whole Person, Not Just the Disease
The COVID-19 pandemic has caused a high level of anxiety and worry across the country and the globe. Heart and Health Medical and the new COVID-19 treatment team is dedicated to providing long-term care and support for our patients and community needs. Our team of diverse medical specialists develops individualized holistic treatment plans for our patients, designed to create the best possible outcomes.
Holistic Post COVID-19 Symptom Care
The treatment and recovery practices of COVID-19 continue to evolve as the medical community learns more about the virus and its long-term effects. For those who have suffered, are suffering, or will suffer from the virus, most symptoms will last for several weeks, but some may experience long-term mild, severe, and sometimes life-threatening damage.
At the Post Covid-19 Recovery Center, we are working with a diverse team of medical specialists to provide comprehensive diagnosis, support, and treatment options for those recovering from long-term Covid-19 symptoms.
Medical Specialty Team Includes:
- Primary Care
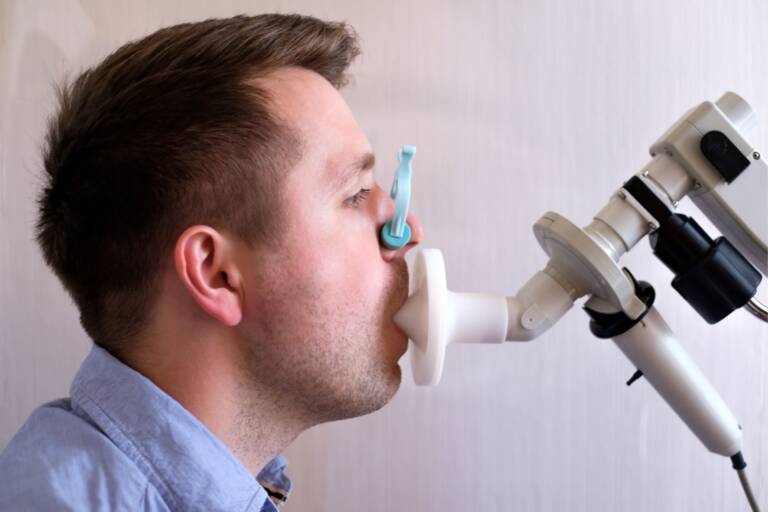
- Pulmonary Medicine
- Cardiology
- Infectious Diseases
- Immunology
- Physical and Occupational Therapy
Long Term Effects of Covid-19
Most people who have mild symptoms of COVID-19 recover completely within a few weeks. But some people continue to experience symptoms after their initial recovery from the virus. Older adults and people with many serious medical conditions are more likely to experience lingering COVID-19 symptoms, but even young, otherwise healthy people can feel unwell for weeks to months after infection. While the less severe symptoms some of the others could lead to health problems in the future, which means constant monitoring and treatments become a priority.
The most common signs and symptoms that linger over time include:
- Cough
- Fatigue
- Shortness of breath
- Joint pain, muscle pain or headache
- Chest pain, fast or pounding heartbeat
- Memory, concentration or sleep problems
- Rash or hair loss
Post COVID-19 Treatment Team
Dr. Matthew Kalter
Board Certified in Pain Management & Physical Medicine and Rehabilitation
Organ damage caused by COVID-19
COVID-19 is an acute respiratory disease that primarily affects the lungs, but it can damage other organs as well. This organ damage may increase the risk of long-term health problems. COVID-19 may cause long term damage in many organs, including:
- The Heart: Imaging tests taken months after recovery from COVID-19 have shown lasting damage to some patients’ heart muscle, even in people who experienced mild to moderate symptoms. This long-term damage may increase the risk of heart failure and other vascular complications in the future.
- The Lungs: The type of pneumonia found in patients suffering from COVID-19 can cause long-standing damage to the tiny air sacs (alveoli) in the lungs, creating permanent scar tissue in the lungs.
- The Brain: COVID-19 has been shown to cause strokes, seizures, and Guillain-Barre syndrome in patients of all ages. COVID-19 may also increase the risk of developing Parkinson’s disease and Alzheimer’s disease.


Blood clots and blood vessel problems
COVID-19 can increase the blood cells’ likelihood to clump up and form clots. There is danger in that large clots can cause heart attacks and strokes. But much of the heart damage caused by COVID-19 is believed to stem from very small clots that block tiny blood vessels (capillaries) in the heart muscle.
COVID-19 can also weaken blood vessels and cause them to leak, which contributes to potentially long-lasting problems with the liver and kidneys. Blood clots in the arteries can cause damage in other parts of the body including the lungs, legs, liver and kidneys.
Problems with fatigue and mood
People who have severe symptoms of COVID-19 often have to be treated in a hospital’s intensive care unit, with mechanical assistance such as ventilators to breathe. Simply surviving this experience can make a person more likely to later develop post-traumatic stress syndrome, depression and anxiety which can be hard to treat with conventional medicines. As with all treatment and recovery practices for COVID-19, treatments for the mental aspects of COVID-19 may continue to evolve as the medical community learns more about the virus and its long-term effect.
Many people who have recovered from SARS have gone on to develop chronic fatigue syndrome, a complex disorder characterized by extreme fatigue that worsens with physical or mental activity but doesn’t improve with rest. The same may be true for people who have had COVID-19.