Osteoporosis: The Silent Bone Thief
Overview of Osteoporosis
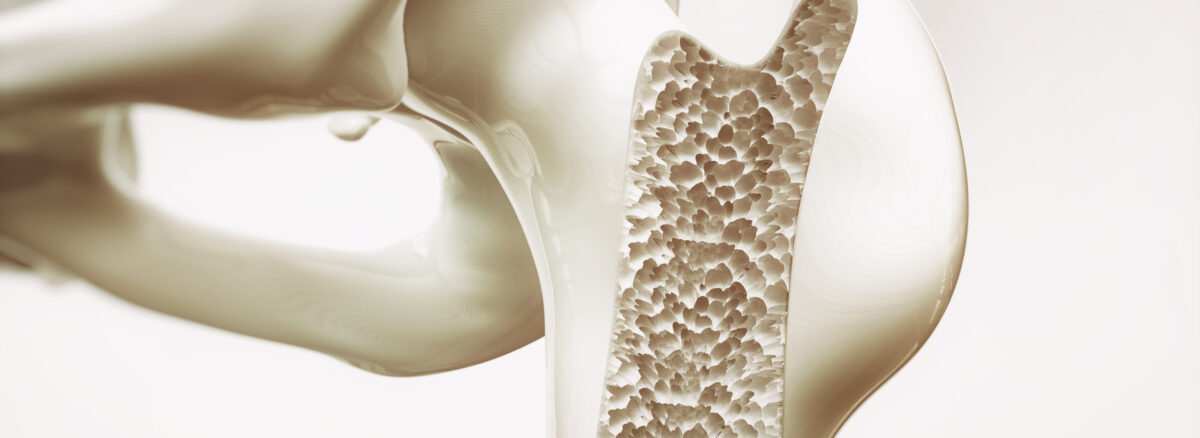
Osteoporosis is a common skeletal disorder characterized by low bone mass, deterioration of bone tissue, and increased risk of fractures. Often referred to as the “silent bone thief,” osteoporosis progresses silently over years, weakening bones and making them more susceptible to fractures, especially in the spine, hips, and wrists.
Osteoporosis primarily affects older adults, particularly postmenopausal women, but can also occur in men and younger individuals. It is a significant public health concern worldwide, contributing to morbidity, mortality, and healthcare costs.
Importance of Bone Health and Endocrinology
Bone health is intricately linked to the endocrine system, which regulates the production and activity of hormones essential for bone formation, remodeling, and maintenance. Hormones such as estrogen, testosterone, parathyroid hormone (PTH), and vitamin D play crucial roles in maintaining bone density and strength.
Endocrine disorders or hormonal imbalances can disrupt bone metabolism, leading to accelerated bone loss and increased risk of osteoporosis. Understanding the interplay between endocrinology and bone health is essential for preventing, diagnosing, and managing osteoporosis effectively.
Understanding Osteoporosis
Definition and Pathophysiology
Osteoporosis is characterized by a gradual weakening of bones, leading to increased susceptibility to fractures. The condition results from an imbalance between bone resorption (the breakdown of old bone tissue) and bone formation (the creation of new bone tissue), tipping the scales in favor of bone loss.
Bone is a dynamic tissue that undergoes constant remodeling, with specialized cells called osteoclasts responsible for breaking down old or damaged bone and osteoblasts responsible for building new bone. In osteoporosis, this balance is disrupted, leading to a net loss of bone mass over time..
Risk Factors for Osteoporosis
Several factors contribute to the development of osteoporosis, including:
- Age and Gender: Osteoporosis is more common in older adults, particularly postmenopausal women, due to hormonal changes that occur during menopause. However, men can also develop osteoporosis, especially with advancing age.
- Hormonal Factors: Hormones such as estrogen and testosterone play key roles in maintaining bone density. Reduced estrogen levels in postmenopausal women and testosterone levels in men can accelerate bone loss.
- Lifestyle Factors: Modifiable lifestyle factors, such as sedentary behavior, smoking, excessive alcohol consumption, and poor nutrition, can contribute to bone loss and increase the risk of osteoporosis.
- Medical Conditions and Medications: Certain medical conditions, such as rheumatoid arthritis, thyroid disorders, and gastrointestinal disorders, can affect bone health. Additionally, long-term use of medications such as corticosteroids, anticonvulsants, and proton pump inhibitors may increase the risk of osteoporosis.
Understanding these risk factors is essential for identifying individuals who may be at higher risk of developing osteoporosis and implementing preventive measures to mitigate their risk. In the following sections, we will explore the role of the endocrine system in bone health and delve into specific hormonal factors that influence bone metabolism and contribute to osteoporosis.
Endocrine System and Bone Health
Role of Hormones in Bone Remodeling
- Estrogen: Estrogen plays a crucial role in maintaining bone density by inhibiting bone resorption and stimulating bone formation. In women, estrogen levels decline significantly after menopause, leading to accelerated bone loss and increased risk of osteoporosis.
- Testosterone: Testosterone, primarily produced in the testes in men and in smaller amounts in the ovaries in women, also contributes to bone health. It promotes bone formation and helps maintain bone density. Low testosterone levels in men, particularly with age, can lead to decreased bone mass and increased fracture risk.
- Parathyroid Hormone (PTH): PTH is produced by the parathyroid glands and plays a vital role in calcium homeostasis. PTH stimulates the release of calcium from bones into the bloodstream when blood calcium levels are low. While PTH is essential for maintaining calcium balance, excessive levels or prolonged exposure to high levels of PTH can lead to bone loss and osteoporosis.
- Vitamin D: Vitamin D is necessary for calcium absorption and utilization in the body. Adequate vitamin D levels are essential for bone mineralization and the prevention of osteoporosis. Deficiency in vitamin D can impair calcium absorption and contribute to bone weakening and increased fracture risk.
Impact of Endocrine Disorders on Bone Health
- Hyperparathyroidism: Hyperparathyroidism, characterized by excessive secretion of PTH, can lead to increased bone resorption and bone loss. Chronic hyperparathyroidism can result in osteoporosis, bone pain, and increased fracture risk.
- Hypogonadism: Hypogonadism, a condition characterized by low levels of sex hormones (e.g., estrogen in women, testosterone in men), can adversely affect bone health. Reduced hormone levels lead to decreased bone formation and increased bone resorption, contributing to osteoporosis.
- Thyroid Disorders: Thyroid hormones, particularly thyroxine (T4) and triiodothyronine (T3), influence bone metabolism. Hyperthyroidism (overactive thyroid) can accelerate bone turnover and increase the risk of osteoporosis, while hypothyroidism (underactive thyroid) can lead to reduced bone formation and bone mineral density.
Causes and Mechanisms of Osteoporosis
Age-Related Bone Loss
Bone Remodeling Changes: As individuals age, the balance between bone resorption and formation becomes disrupted, leading to a gradual loss of bone density. This age-related bone loss, known as primary osteoporosis, occurs more rapidly in women after menopause due to declining estrogen levels.
Decreased Bone Formation: With advancing age, osteoblast activity declines, resulting in reduced bone formation. This contributes to the overall decrease in bone density and strength observed in older adults.
Hormonal Changes and Imbalances
- Estrogen Deficiency: Declining estrogen levels, particularly during menopause in women, lead to accelerated bone loss. Estrogen plays a vital role in inhibiting bone resorption and stimulating bone formation. Reduced estrogen levels result in increased bone turnover and a higher risk of osteoporosis-related fractures.
- Testosterone Deficiency: Low testosterone levels in men, often associated with aging, can also contribute to bone loss and osteoporosis. Testosterone plays a role in promoting bone formation and maintaining bone density. Decreased testosterone levels lead to decreased osteoblast activity and increased bone resorption, predisposing men to osteoporotic fractures.
Nutritional Deficiencies
Calcium and Vitamin D Deficiency: Inadequate intake of calcium and vitamin D can impair bone mineralization and weaken bones. Calcium is essential for bone structure, while vitamin D facilitates calcium absorption in the intestines. Deficiencies in these nutrients can lead to decreased bone density and an increased risk of osteoporosis.
Sedentary Lifestyle and Lack of Exercise
Decreased Mechanical Loading: Physical activity and weight-bearing exercise stimulate bone formation and help maintain bone density. A sedentary lifestyle or lack of exercise can lead to decreased mechanical loading on bones, resulting in reduced bone strength and increased susceptibility to fractures.
Genetics and Family History
Genetic Factors: Genetic predisposition plays a role in determining an individual’s risk of osteoporosis. Family history of osteoporosis or fragility fractures may increase an individual’s susceptibility to the condition.
Diagnosis and Screening for Osteoporosis
Bone Density Testing (DXA Scan)
Dual-Energy X-ray Absorptiometry (DXA): DXA scanning is the most commonly used method for measuring bone mineral density (BMD) and diagnosing osteoporosis. It uses low-dose X-rays to assess bone density at key sites, such as the hip and spine. Results are reported as T-scores, which compare an individual’s BMD to that of a healthy young adult of the same sex.
Screening Recommendations: The National Osteoporosis Foundation (NOF) recommends DXA screening for:
- Women aged 65 and older
- Men aged 70 and older
- Younger individuals with risk factors for osteoporosis, such as a history of fragility fractures, long-term corticosteroid use, or certain medical conditions
Fracture Risk Assessment
- Fracture Risk Calculators: Various fracture risk assessment tools, such as the FRAX (Fracture Risk Assessment Tool), use clinical risk factors along with BMD measurements to estimate an individual’s 10-year probability of major osteoporotic fractures (e.g., hip, spine, wrist) and hip fractures. These tools help guide clinical decision-making regarding osteoporosis diagnosis and treatment.
- Clinical Risk Factors: Factors such as age, sex, previous fragility fractures, parental history of hip fracture, smoking, alcohol intake, and glucocorticoid use are taken into account when assessing fracture risk.
Screening Guidelines and Recommendations
Guidelines by Professional Organizations: Professional organizations, such as the American College of Physicians (ACP), the U.S. Preventive Services Task Force (USPSTF), and the International Society for Clinical Densitometry (ISCD), provide recommendations for osteoporosis screening and management based on age, risk factors, and clinical judgment.
Individualized Approach: Screening recommendations may vary based on individual risk factors, preferences, and overall health status. Healthcare providers should consider a patient’s age, sex, fracture risk, and other clinical factors when determining the need for osteoporosis screening.
Early detection of osteoporosis through bone density testing and fracture risk assessment allows for timely intervention and management to prevent fractures and reduce morbidity. In the following section, we will explore treatment options and management strategies for osteoporosis, aimed at preserving bone health and reducing fracture risk.
Treatment Options for Osteoporosis
Pharmacological Interventions
Bisphosphonates: Bisphosphonates are commonly prescribed medications for the treatment of osteoporosis. They work by inhibiting bone resorption, thereby slowing down bone loss and reducing fracture risk. Examples of bisphosphonates include alendronate, risedronate, ibandronate, and zoledronic acid.
Selective Estrogen Receptor Modulators (SERMs): SERMs, such as raloxifene, mimic the effects of estrogen on bone tissue. They help maintain bone density and reduce fracture risk in postmenopausal women without the risks associated with hormone replacement therapy (HRT).
Monoclonal Antibody Therapy: Monoclonal antibody therapy, such as denosumab, targets a protein called RANK ligand, which plays a key role in bone resorption. By inhibiting RANK ligand, denosumab reduces bone turnover and increases bone density, thereby reducing fracture risk.
Lifestyle Modifications
Exercise Programs: Weight-bearing and resistance exercises help strengthen bones and improve balance, reducing the risk of falls and fractures. Incorporating exercises such as walking, jogging, strength training, and balance exercises into a regular exercise routine can help preserve bone health.
Dietary Changes: A diet rich in calcium and vitamin D is essential for maintaining bone health. Calcium-rich foods include dairy products, leafy green vegetables, and fortified foods. Vitamin D can be obtained from fatty fish, fortified dairy products, and sunlight exposure. In cases of inadequate dietary intake, supplements may be recommended.
Fall Prevention Strategies: Implementing fall prevention measures, such as removing tripping hazards, improving lighting in the home, and using assistive devices as needed, can reduce the risk of falls and fractures, especially in older adults.
Medical Management
Regular Monitoring and Follow-Up: Individuals with osteoporosis should undergo regular monitoring of bone density and fracture risk, as well as periodic evaluation of treatment efficacy and side effects. Adjustments to treatment may be made based on changes in bone density and fracture risk over time.
Multidisciplinary Approach: Managing osteoporosis often requires a multidisciplinary approach involving healthcare providers such as primary care physicians, endocrinologists, rheumatologists, orthopedic surgeons, physical therapists, and dietitians. Collaborative care ensures comprehensive evaluation, treatment, and management of osteoporosis and related complications.
By combining pharmacological interventions, lifestyle modifications, and medical management, individuals with osteoporosis can effectively manage the condition, preserve bone health, and reduce fracture risk. In the next section, we will explore the management of osteoporosis in the context of endocrine disorders and provide recommendations for promoting overall bone health.