Angina
Angina (an-JI-nuh or AN-juh-nuh) is chest pain or discomfort that occurs when an area of your heart muscle doesn’t get enough oxygen-rich blood. Angina may feel like pressure or squeezing in your chest. The pain also may occur in your shoulders, arms, neck, jaw, or back. It can feel like indigestion.
Angina itself isn’t a disease. Rather, it’s a symptom of an underlying heart problem. Angina is usually a symptom of coronary artery disease (CAD), the most common type of heart disease.
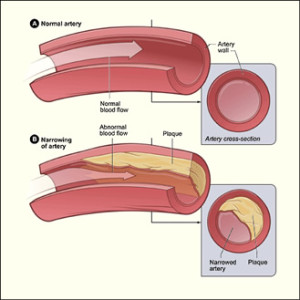
CAD occurs when a fatty material called plaque (plak) builds up on the inner walls of the coronary arteries. These arteries carry oxygen-rich blood to your heart. When plaque builds up in the arteries, the condition is called atherosclerosis (ATH-er-o-skler-O-sis).
Plaque causes the coronary arteries to become narrow and stiff. The flow of oxygen-rich blood to the heart muscle is reduced. This causes pain and can lead to a heart attack.
Types of Angina
The three types of angina are stable, unstable, and variant (Prinzmetal’s). Knowing how the types are different is important. This is because they have different symptoms and require different treatment.
Stable Angina
Stable angina is the most common type. It occurs when the heart is working harder than usual. Stable angina has a regular pattern. If you know you have stable angina, you can learn to recognize the pattern and predict when the pain will occur.
The pain usually goes away in a few minutes after you rest or take your angina medicine.
Stable angina isn’t a heart attack, but it makes a heart attack more likely in the future.
Unstable Angina
Unstable angina doesn’t follow a pattern. It can occur with or without physical exertion and isn’t relieved by rest or medicine.
Unstable angina is very dangerous and needs emergency treatment. It’s a sign that a heart attack may happen soon.
Variant (Prinzmetal’s) Angina
Variant angina is rare. It usually occurs while you’re at rest. The pain can be severe. It usually happens between midnight and early morning. This type of angina is relieved by medicine.
Overview of CAD
It’s thought that nearly 7 million people in the United States suffer from angina. About 400,000 patients go to their doctors with new cases of angina every year.
Angina occurs equally in men and women. It can be a sign of heart disease, even when initial tests don’t show evidence of CAD.
Not all chest pain or discomfort is angina. A heart attack, lung problems (such as an infection or a blood clot), heartburn, or a panic attack also can cause chest pain or discomfort. All chest pain should be checked by a doctor.

Signs and Symptoms
Pain and discomfort are the main symptoms of angina. Angina is often described as pressure, squeezing, burning, or tightness in the chest. It usually starts in the chest behind the breastbone.
Pain from angina also can occur in the arms, shoulders, neck, jaw, throat, or back. It may feel like indigestion.
Some people say that angina discomfort is hard to describe or that they can’t tell exactly where the pain is coming from.
Symptoms such as nausea (feeling sick to your stomach), fatigue (tiredness), shortness of breath, sweating, light-headedness, or weakness also may occur. Women are more likely to feel is comfort in their back, shoulders, and abdomen.
Symptoms vary based on the type of angina.
Stable Angina
The pain or discomfort:
- Occurs when the heart must work harder, usually during physical exertion
- Doesn’t come as a surprise, and episodes of pain tend to be alike
- Usually lasts a short time (5 minutes or less)
- Is relieved by rest or medicine
- May feel like gas or indigestion
- May feel like chest pain that spreads to the arms, back, or other areas
Unstable Angina
The pain or discomfort:
- Often occurs at rest, while sleeping at night, or with little physical exertion
- Comes as a surprise
- Is more severe and lasts longer (as long as 30 minutes) than episodes of stable angina
- Is usually not relieved with rest or medicine
- May get continually worse
- May mean that a heart attack will happen soon
Variant Angina
The pain or discomfort:
- Usually occurs at rest and during the night or early morning hours
- Tends to be severe
- Is relieved by medicine
Lasting Chest Pain
Chest pain that lasts longer than a few minutes and isn’t relieved by rest or angina medicine may mean you’re having (or are about to have) a heart attack. Call 9–1–1 right away.
Angina Diagnosis
The most important issues to address when you go to the doctor with chest pain are:
- What’s causing the chest pain
- Whether you’re having or are about to have a heart attack
Angina is a symptom of an underlying heart problem, usually coronary artery disease (CAD). The type of angina pain you have can be a sign of how severe the CAD is and whether it’s likely to cause a heart attack.
If you have chest pain, your doctor will want to find out whether it’s angina. He or she also will want to know whether the angina is stable or unstable. If it’s unstable, you may need emergency medical attention to try to prevent a heart attack.
To diagnose chest pain as stable or unstable angina, your doctor will do a physical exam, ask about your symptoms, and ask about your risk factors and your family history of CAD or other heart disease.
He or she may also ask questions about your symptoms, such as:
- What brings on the pain or discomfort and what relieves it?
- What does the pain or discomfort feel like (for example, heaviness or tightness)?
- How often does the pain occur?
- Where do you feel the pain or discomfort?
- How severe is the pain or discomfort?
- How long does the pain or discomfort last?

Diagnostic Tests and Procedures
If your doctor suspects that you have unstable angina or that your angina is related to a serious heart condition, he or she may order one or more tests.
EKG (Electrocardiogram)
An EKG is a simple test that detects and records the electrical activity of your heart. An EKG shows how fast your heart is beating and whether it has a regular rhythm. It also shows the strength and timing of electrical signals as they pass through each part of your heart.
Certain electrical patterns that the EKG detects can suggest whether CAD is likely. An EKG also can show signs of a previous or current heart attack.
However, some people with angina have a normal EKG.
Stress Testing
During stress testing, you exercise to make your heart work hard and beat fast while heart tests are performed. If you can’t exercise, you’re given medicine to speed up your heart rate.
During exercise stress testing, your blood pressure and EKG readings are checked while you walk or run on a treadmill or pedal a bicycle. Other heart tests, such as nuclear heart scanning or echocardiography, also can be done at the same time.
If you’re unable to exercise, a medicine can be injected into your bloodstream to make your heart work hard and beat fast. Nuclear heart scanning or echocardiography is then usually done.
When your heart is beating fast and working hard, it needs more blood and oxygen. Arteries narrowed by plaque can’t supply enough oxygen-rich blood to meet your heart’s needs.
A stress test can show possible signs of CAD, such as:
- Abnormal changes in your heart rate or blood pressure
- Symptoms such as shortness of breath or chest pain
- Abnormal changes in your heart rhythm or your heart’s electrical activity
Chest X Ray
A chest x ray takes a picture of the organs and structures inside the chest, including your heart, lungs, and blood vessels. A chest x ray can reveal signs of heart failure, as well as lung disorders and other causes of symptoms that aren’t due to CAD.
Coronary Angiography and Cardiac Catheterization
Your doctor may ask you to have coronary angiography (an-jee-OG-ra-fee) if other tests or factors show that you’re likely to have CAD. This test uses dye and special x rays to show the insides of your coronary arteries.
To get the dye into your coronary arteries, your doctor will use a procedure called cardiac catheterization (KATH-e-ter-i-ZA-shun). A long, thin, flexible tube called a catheter is put into a blood vessel in your arm, groin (upper thigh), or neck. The tube is then threaded into your coronary arteries, and the dye is released into your bloodstream. Special x rays are taken while the dye is flowing through the coronary arteries.
Cardiac catheterization is usually done in a hospital. You’re awake during the procedure. It usually causes little to no pain, although you may feel some soreness in the blood vessel where your doctor put the catheter.
Blood Tests
Blood tests check the levels of certain fats, cholesterol, sugar, and proteins in your blood. Abnormal levels may show that you have risk factors for CAD.Your doctor may order a blood test to check the level of C-reactive protein (CRP) in your blood. Some studies suggest that high levels of CRP in the blood may increase the risk for CAD and heart attack. Your doctor also may order a blood test to check for low hemoglobin (HEE-muh-glow-bin) in your blood. Hemoglobin is an iron-rich protein in the red blood cells that carries oxygen from the lungs to all parts of your body. If you have low hemoglobin, you may have a condition called anemia (uh-NEE-me-eh).
Treatments For Angina
Treatments for angina include lifestyle changes, medicines, medical procedures, and cardiac rehabilitation (rehab). The main goals of treatment are to:
- Reduce pain and discomfort and how often it occurs
- Prevent or lower the risk of heart attack and death by treating the underlying heart condition
Lifestyle changes and medicines may be the only treatments needed if your symptoms are mild and aren’t getting worse. When lifestyle changes and medicines don’t control angina, you may need medical procedures or cardiac rehab.
Unstable angina is an emergency condition that requires treatment in the hospital.
Lifestyle Changes
Making lifestyle changes can help prevent episodes of angina. You can:
- Slow down or take rest breaks if angina comes on with exertion.
- Avoid large meals and rich foods that leave you feeling stuffed if angina comes on after a heavy meal.
- Try to avoid situations that make you upset or stressed if angina comes on with stress. Learn ways to handle stress that can’t be avoided.
You also can make lifestyle changes that help lower your risk of heart disease. An important lifestyle change is adopting a healthy diet. This will help prevent or reduce high blood pressure, high blood cholesterol, and obesity.

Follow a heart healthy eating plan that focuses on fruits, vegetables, whole grains, low-fat or no-fat diary products, and lean meat and fish. The plan also should be low in alt, fat, saturated fat, trans fat, and cholesterol.
Examples of healthy eating plans are the National Heart, Lung, and Blood Institute’s Therapeutic Lifestyle Changes (TLC) diet and the Dietary Approaches to Stop Hypertension (DASH) eating plan.
Your doctor may recommend TLC if you have high cholesterol or the DASH eating plan if you have high blood pressure. Even if you don’t have these conditions, you can still benefit from these heart healthy plans.
Other important lifestyle changes include:
Quitting smoking, if you smoke. Avoid secondhand smoke.
Being physically active. Check with your doctor to find out how much and what kinds of activity are safe for you.
Losing weight, if you’re overweight or obese.
Taking all medicines as your doctor prescribes, especially if you have diabetes.
Angina Medicines
Nitrates are the most commonly used medicines to treat angina. They relax and widen blood vessels. This allows more blood to flow to the heart while reducing its workload.
Nitroglycerin is the most commonly used nitrate for angina. Nitroglycerin that dissolves under your tongue or between your cheeks and gum is used to relieve an angina episode. Nitroglycerin in the form of pills and skin patches is used to prevent attacks of angina. These forms of nitroglycerin act too slowly to relieve pain during an angina attack.
You also may need other medicines to treat angina. These medicines may include beta blockers, calcium channel blockers, ACE inhibitors, oral antiplatelet (an-ty-PLAYT-lit) medicines, and anticoagulants (AN-te-ko-AG-u-lants). These medicines can help:
- Lower blood pressure and cholesterol levels
- Slow the heart rate
- Relax blood vessels
- Reduce strain on the heart
- Prevent blood clots from forming
Medical Procedures
When medicines and other treatments don’t control angina, you may need a medical procedure to treat the underlying heart disease. Angioplasty (AN-jee-oh-plas-tee) and coronary artery bypass grafting (CABG) are both commonly used to treat angina.
Angioplasty opens blocked or narrowed coronary arteries. During angioplasty, a thin tube with a balloon or other device on the end is threaded through a blood vessel to the narrowed or blocked coronary artery. Once in place, the balloon is inflated to push the plaque outward against the wall of the artery. This widens the artery and restores blood flow.
Angioplasty can improve blood flow to your heart, relieve chest pain, and possibly prevent a heart attack. Sometimes a small mesh tube called a stent is placed in the artery to keep it open after the procedure.
During CABG, healthy arteries or veins taken from other areas in your body are used to bypass (that is, go around) your narrowed coronary arteries. Bypass surgery can improve blood flow to your heart, relieve chest pain, and possibly prevent a heart attack.
Your doctor will help decide which treatment is right for you.
Cardiac Rehabilitation
Your doctor may prescribe cardiac rehab for angina or after angioplasty, CABG, or a heart attack.
The cardiac rehab team may include doctors, nurses, exercise specialists, physical and occupational therapists, dietitians, and psychologists or other behavioral therapists.
Rehab has two parts:
- Exercise training. This part helps you learn how to exercise safely, strengthen your muscles, and improve your stamina. Your exercise plan will be based on your individual abilities, needs, and interests.
- Education, counseling, and training. This part of rehab helps you understand your heart condition and find ways to reduce your risk of future heart problems. The cardiac rehab team will help you learn how to cope with the stress of adjusting to a new lifestyle and to deal with your fears about the future.

