Atherosclerosis
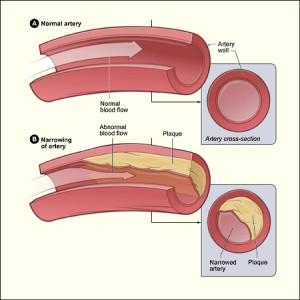
Atherosclerosis (ath-er-o-skler-O-sis) is a disease in which plaque (plak) builds up inside your arteries. Arteries are blood vessels that carry oxygen-rich blood to your heart and other parts of your body.
Plaque is made up of fat, cholesterol, calcium, and other substances found in the blood. Over time, plaque hardens and narrows your arteries, limiting the flow of oxygen-rich blood to your organs and other parts of your body. This can lead to severe problems, including heart attack, stroke, or even death.
Atherosclerosis-Related Diseases
Atherosclerosis can affect any artery in the body, including arteries in the heart, brain, arms, legs, and pelvis. As a result, different diseases may develop based on which arteries are affected.
Coronary Heart Disease
Coronary heart disease (CHD) occurs if plaque builds up in the coronary arteries. These arteries supply oxygen-rich blood to your heart.
Plaque narrows the coronary arteries and reduces blood flow to your heart muscle. It also makes it more likely that blood clots will form in your arteries. Blood clots can partially or completely block blood flow.
When blood flow to your heart muscle is reduced or blocked, it can lead to angina (chest pain) and a heart attack. CHD also is called coronary artery disease or heart disease. It’s the leading cause of death for both men and women in the United States.
Plaque also can form in the heart’s smallest arteries. When this happens, it’s called coronary microvascular disease (MVD). In coronary MVD, plaque doesn’t always cause blockages in the arteries as it does in CHD.
Carotid Artery Disease
Carotid (ka-ROT-id) artery disease occurs if plaque builds up in the arteries on each side of your neck. These arteries supply oxygen-rich blood to your brain. When blood flow to your brain is reduced or blocked, it can lead to a stroke.
Peripheral Arterial Disease
Peripheral arterial disease (P.A.D.) occurs if plaque builds up in the major arteries that supply oxygen-rich blood to your legs, arms, and pelvis.
When blood flow to these parts of your body is reduced or blocked, it can lead to numbness, pain, and, sometimes, dangerous infections.
Atherosclerosis Overview
The cause of atherosclerosis isn’t known. However, certain traits, conditions, or habits may raise your risk for the disease. These conditions are known as risk factors.
You can control some risk factors, such as lack of physical activity, smoking, and an unhealthy diet, others you can’t control, such as age and a family history of heart disease.
Some people who have atherosclerosis have no signs or symptoms. They may not be diagnosed until after a heart attack or stroke.
The primary treatment for atherosclerosis is lifestyle changes. You also may need medicines and medical procedures. These treatments, along with ongoing medical care, can help you live a healthier life.
Atherosclerosis Outlook
Better treatments have reduced the number of deaths from atherosclerosis-related diseases. These treatments also have improved the quality of life for people who have these diseases. However, atherosclerosis remains a common health problem.
You may be able to prevent or delay atherosclerosis and the diseases it can cause. Making lifestyle changes and getting ongoing care can help you avoid the problems of atherosclerosis and live a long, healthy life.
Signs and Symptoms of Atherosclerosis
Atherosclerosis usually doesn’t cause signs and symptoms until it severely narrows or totally blocks an artery. Many people don’t know they have the disease until they have a medical emergency, such as a heart attack or stroke.
Coronary Arteries
The coronary arteries supply oxygen-rich blood to your heart. When plaque narrows or blocks these arteries (a condition called coronary heart disease or CHD), a common symptom is angina. Angina is chest pain or discomfort that occurs when your heart muscle doesn’t get enough oxygen-rich blood.
Angina may feel like pressure or a squeezing pain in your chest. You also may feel it in your shoulders, arms, neck, jaw, or back. This pain tends to get worse with activity and goes away when you rest. Emotional stress also can trigger the pain.
Other symptoms of CHD are shortness of breath and arrhythmias (ah-RITH-me-ahs). Arrhythmias are problems with the rate or rhythm of the heartbeat.
Plaque also can form in the heart’s smallest arteries. When this happens, it’s called coronary microvascular disease (MVD). In addition to angina and shortness of breath, coronary MVD also may cause sleep problems, fatigue (tiredness), and lack of energy.
Carotid Arteries
The carotid arteries supply oxygen-rich blood to your brain. When plaque narrows or blocks these arteries (a condition called carotid artery disease), you may have symptoms of a stroke. These symptoms may include:
- Sudden weakness or numbness in the face or limbs, often on just one side of the body
- The inability to move one or more of your limbs
- Trouble speaking and understanding
- Sudden trouble seeing in one or both eyes
- Dizziness or loss of balance
- A sudden, severe headache with no known cause
Peripheral Arteries
Plaque also can build up in the major arteries that supply oxygen-rich blood to the legs, arms, and pelvis. When this happens, it’s called peripheral arterial disease. If these major arteries are narrowed or blocked, it can lead to numbness, pain, and, sometimes, dangerous infections.
Diagnosing Atherosclerosis
Your doctor will diagnose atherosclerosis based on your medical and family histories, a physical exam, and results from tests.
Specialists Involved
If you have atherosclerosis, a primary care doctor, such as an internist or family practitioner, may handle your care. Your doctor may recommend other health care specialists if you need expert care. These specialists may include:
- Cardiologist, a doctor who specializes in diagnosing and treating heart diseases and conditions. You may see a cardiologist if you have coronary heart disease (CHD) or coronary microvascular disease (MVD).
- Vascular specialist, a doctor who specializes in diagnosing and treating blood vessel problems. You may see a vascular specialist if you have peripheral arterial disease (P.A.D.).
- Neurologist, a doctor who specializes in diagnosing and treating nervous system disorders. You may see a neurologist if you’ve had a stroke due to carotid artery disease.

Physical Exam
During the physical exam, your doctor may listen to your arteries for an abnormal whooshing sound called a bruit (broo-E). Your doctor can hear a bruit when placing a stethoscope over an affected artery. A bruit may indicate poor blood flow due to plaque buildup.
Your doctor may also check to see if your pulse (for example, in the leg or foot) is weak or absent. A weak or absent pulse can be a sign of a blocked artery.
Diagnostic Tests
Your doctor may recommend one or more tests to diagnose atherosclerosis. These tests also can help your doctor learn the extent of your disease and plan the best treatment.
Blood Tests
Blood tests check the levels of certain fats, cholesterol, sugar, and proteins in your blood. Abnormal levels may be a sign that you’re at risk for atherosclerosis.
EKG (Electrocardiogram)
An EKG is a simple, painless test that detects and records the heart’s electrical activity. The test shows how fast the heart is beating and its rhythm (steady or irregular). An EKG also records the strength and timing of electrical signals as they pass through each part of the heart.
An EKG can show evidence of heart damage due to CHD and signs of a previous or current heart attack.
Chest X-Ray
A chest x-ray takes pictures of the organs and structures inside your chest, such as your heart, lungs, and blood vessels. A chest x-ray can reveal signs of heart failure.
Ankle/Brachial Index
This test compares the blood pressure in your ankle with the blood pressure in your arm to see how well your blood is flowing. This test can help diagnose P.A.D.
Echocardiography
Echocardiography (echo) uses sound waves to create a moving picture of your heart. The test provides information about the size and shape of your heart and how well your heart chambers and valves are working.
Echo also can identify areas of poor blood flow to the heart, areas of the heart muscle that aren’t contracting normally, and previous injury to the heart muscle caused by poor blood flow.
Computed Tomography Scan
A computed tomography (CT) scan creates computer-generated pictures of the heart, brain, or other areas of the body. The test often can show hardening and narrowing of large arteries.
A CT scan also can show whether calcium has built up in the walls of the coronary (heart) arteries, this may be an early sign of CHD.
Stress Testing
During stress testing, you exercise (or are given medicine if you are unable to exercise) to make your heart work hard and beat fast while heart tests are done.
When your heart is working hard and beating fast, it needs more blood and oxygen. Plaque-narrowed arteries can’t supply enough oxygen-rich blood to meet your heart’s needs.
A stress test can show possible signs and symptoms of CHD, such as:
- Abnormal changes in your heart rate or blood pressure
- Shortness of breath or chest pain
- Abnormal changes in your heart rhythm or your heart’s electrical activity
As part of some stress tests, pictures are taken of your heart while you exercise, and while you rest. These imaging stress tests can show how well blood is flowing in various parts of your heart and/or how well your heart squeezes out blood when it beats.
Angiography
Angiography (an-jee-OG-ra-fee) is a test that uses dye and special x rays to show the insides of your arteries. This test can show whether plaque is blocking your arteries and how severe the blockage is.
A thin, flexible tube called a catheter is put into a blood vessel in your arm, groin (upper thigh), or neck. A dye that can be seen on an x-ray is then injected through the catheter into the arteries. By looking at the x-ray picture, your doctor can see the flow of blood through your arteries.
Treatment of Atherosclerosis
Treatments for atherosclerosis may include lifestyle changes, medicines, and medical procedures or surgery.
The goals of treatment include:
- Relieving symptoms
- Reducing risk factors in an effort to slow or stop the buildup of plaque
- Lowering the risk of blood clots forming
- Widening or bypassing plaque-clogged arteries
- Preventing atherosclerosis-related diseases

Lifestyle Changes
Making lifestyle changes often can help prevent or treat atherosclerosis. For some people, these changes may be the only treatment needed.
Follow a Healthy Diet
A healthy diet is an important part of a healthy lifestyle. Following a healthy diet can prevent or reduce high blood pressure and high blood cholesterol and help you maintain a healthy weight.
For information on healthy eating, go to the National Heart, Lung, and Blood Institute’s (NHLBI’s) Aim for a Healthy Weight Web site. This site provides practical tips on healthy eating, physical activity, and controlling your weight.
Therapeutic Lifestyle Changes (TLC).
Your doctor may recommend TLC if you have high blood cholesterol. TLC is a three-part program that includes a healthy diet, physical activity, and weight management.
With the TLC diet, less than 7 percent of your daily calories should come from saturated fat. This kind of fat is found in some meats, dairy products, chocolate, baked goods, and deep-fried and processed foods.
No more than 25 to 35 percent of your daily calories should come from all fats, including saturated, trans, monounsaturated, and polyunsaturated fats.
You also should have less than 200 mg a day of cholesterol. The amounts of cholesterol and the types of fat in prepared foods can be found on the foods’ Nutrition Facts labels.
Foods high in soluble fiber also are part of a healthy diet. They help prevent the digestive tract from absorbing cholesterol. These foods include:
- Whole-grain cereals such as oatmeal and oat bran
- Fruits such as apples, bananas, oranges, pears, and prunes
- Legumes such as kidney beans, lentils, chickpeas, black-eyed peas, and lima beans
A diet rich in fruits and vegetables can increase important cholesterol-lowering compounds in your diet. These compounds, called plant stanols or sterols, work like soluble fiber.
A healthy diet also includes some types of fish, such as salmon, tuna (canned or fresh), and mackerel. These fish are a good source of omega-3 fatty acids. These acids may help protect the heart from blood clots and inflammation and reduce the risk of a heart attack. Try to have about two fish meals every week.
You also should try to limit the amount of sodium (salt) that you eat. This means choosing low-salt and “no added salt” foods and seasonings at the table or when cooking. The Nutrition Facts label on food packaging shows the amount of sodium in the item.
Try to limit drinks with alcohol. Too much alcohol will raise your blood pressure and triglyceride level. (Triglycerides are a type of fat found in the blood.) Alcohol also adds extra calories, which will cause weight gain.
Men should have no more than two drinks containing alcohol a day. Women should have no more than one drink containing alcohol a day. One drink is a glass of wine, beer, or a small amount of hard liquor.
For more information about TLC, see the NHLBI’s “Your Guide to Lowering Your Cholesterol With TLC.”
Dietary Approaches to Stop Hypertension (DASH).
Your doctor may recommend the DASH eating plan if you have high blood pressure. The DASH eating plan focuses on fruits, vegetables, whole grains, and other foods that are heart-healthy and low in fat, cholesterol, and salt.
DASH also focuses on fat-free or low-fat milk and dairy products, fish, poultry, and nuts. The DASH eating plan is reduced in red meat (including lean red meat), sweets, added sugars, and sugar-containing beverages. It’s rich in nutrients, protein, and fiber.
The DASH eating plan is a good heart-healthy eating plan, even for those who don’t have high blood pressure. For more information, see the NHLBI’s “Your Guide to Lowering Your Blood Pressure With DASH.”
Do Physical Activity Regularly
Regular physical activity can lower many atherosclerosis risk factors, including LDL (“bad”) cholesterol, high blood pressure, and excess weight.
Physical activity also can lower your risk of diabetes and raise your HDL cholesterol level. HDL is the “good” cholesterol that helps prevent atherosclerosis.
Talk to your doctor before you start a new exercise plan. Ask him or her how much and what kinds of physical activity are safe for you.
People gain health benefits from as little as 60 minutes of moderate-intensity aerobic activity per week. The more active you are, the more you will benefit.

For more information on physical activity, see the U.S. Department of Health and Human Services’ “2008 Physical Activity Guidelines for Americans,” the Diseases and Conditions Index Physical Activity and Your Heart article, and the NHLBI’s “Your Guide to Physical Activity and Your Heart.”
Maintain a Healthy Weight
Maintaining a healthy weight can lower your risk of atherosclerosis. A general goal to aim for is a body mass index (BMI) of less than 25.
BMI measures your weight in relation to your height and gives an estimate of your total body fat. You can use the NHLBI’s online BMI calculator to figure out your BMI, or your doctor can help you.
A BMI between 25 and 29.9 is considered overweight. A BMI of 30 or more is considered obese. A BMI of less than 25 is the goal for preventing and treating atherosclerosis. Your doctor or other health care provider can help you set an appropriate goal for you.
For more information on losing weight and maintaining your weight, see the Diseases and Conditions Index Overweight and Obesity article.
Quit Smoking
If you smoke or use tobacco, quit. Smoking can damage and tighten blood vessels and raise your risk of atherosclerosis.
Talk to your doctor about programs and products that can help you quit. Also, try to avoid secondhand smoke. For more information on how to quit smoking, see the NHLBI’s “Your Guide to a Healthy Heart.”
Manage Stress
Research shows that the most commonly reported “trigger” for a heart attack is an emotionally upsetting event—particularly one involving anger. Also, some of the ways people cope with stress, such as drinking, smoking, or overeating, aren’t healthy.
Learning how to manage stress, relax, and cope with problems can improve your emotional and physical health. Having supportive people in your life with whom you can share your feelings or concerns can help relieve stress.
Physical activity, medicine, and relaxation therapy also can help relieve stress. You may want to consider participating in a stress management program.
Medicines
To slow the progress of plaque buildup, your doctor may prescribe medicines to help lower your cholesterol level or blood pressure or to prevent blood clots from forming.
For successful treatment, take all medicines as your doctor prescribes.
Medical Procedures and Surgery
If you have severe atherosclerosis, your doctor may recommend one of several procedures or surgeries.
Angioplasty is a procedure that’s used to open blocked or narrowed coronary (heart) arteries. Angioplasty can improve blood flow to the heart, relieve chest pain, and possibly prevent a heart attack. Sometimes a small mesh tube called a stent is placed in the artery to keep it open after the procedure.
Coronary artery bypass grafting (CABG) is a type of surgery. In CABG, arteries or veins from other areas in your body are used to bypass (that is, go around) your narrowed coronary arteries. CABG can improve blood flow to your heart, relieve chest pain, and possibly prevent a heart attack.
Bypass grafting also can be used for leg arteries. In this surgery, a healthy blood vessel is used to bypass a narrowed or blocked artery in one of your legs. The healthy blood vessel redirects blood around the artery, improving blood flow to the leg.
Carotid endarterectomy (END-ar-ter-EK-to-me), or carotid artery surgery, removes plaque buildup from the carotid arteries in the neck. This procedure opens the arteries and improves blood flow to the brain, which can help prevent a stroke.


