Asthma Specialists
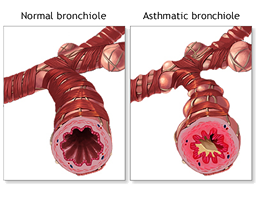
Our Asthma specialists are dedicated to helping treat the source of any type of allergy. Our offices are conveniently located in Nassau and Suffolk County in Long Island, NY. Asthma is a medical condition that results in the narrowing and swelling of the lung’s airways. Since these airways become restricted, common symptoms of asthma are shortness of breath, wheezing, and chest tightness. During an asthma attack, the lining of the airways tightens and narrows, therefore reducing the amount of air passage.
Cells in the aviation routes may make more bodily fluid than typical. (Bodily fluid is a sticky, thick fluid that can further limit your aviation routes.)
This chain response can bring about asthma indications. Indications may incorporate wheezing (a shrieking sound when you inhale), midsection snugness, shortness of breath, and hacking.
It’s vital to treat side effects when you first notice them. This will help keep the manifestations from intensifying and bringing on an extreme asthma attack. Serious asthma attacks may require more attention, or they might result in a high risk of fatality.
What is Asthma
Asthma is an obstructive lung disease that causes a narrowing of the airways. The blockage of airways causes patchiness in lung ventilation that intensifies with expiration. Additionally, asthma is a progressive disease that typically worsens overtime. There is no real cure, however, asthma can be managed and treated.
If the asthma cannot be reversed even after administration of a drug treatment it is known as severe asthma. Severe asthma has constant airflow limitation and localized atelectasis. Atelectasis occurs when there is a buildup of fluid and no air in a part of the lung. This causes a collapse in the lungs and leads to an imminent death.
Asthma Symptoms
Symptoms vary day to day, time of day, seasonal, or during life stages. Though, they are commonly worse at night or early morning.
- Dyspnea
- Chest tightness
- Wheezes (rhonchi)
- Coughing
- Eczema (red/itchy skin)
- Associated with allergies (Allergy-Induced Asthma)
Why does this happen?
ACh contracts and relaxes the smooth muscles in the walls of the airway of a healthy individual. Individuals with asthma have hyperresponsiveness of ACh, which constantly contracts the smooth muscles. The physical stimulation can cause bronchoconstriction, bronchospasm, and coughing.
The thickened basement membrane is a hallmark for asthma causing an inflammation-induced chemical stimulation of the cells. The increase in goblet cell differentiation causes an accumulation of mucus secretion. The mucus produced is rubberier and more vicious than a healthy individual creating resistance. In a healthy individual, the cilia in the airway propels the mucus away from the alveoli in the lungs and towards the mouth. Cilia are hair-like organelles that extend from the cell body into the surrounding fluid. In asthma patients, cilia cannot sweep up the mucus due to the rubbery texture, which results in a blockage of the airway.
Additionally, the hyperplasia and hypertrophy worsen the bronchoconstriction by thickening the airway walls. Hyperplasia is an increased amount of smooth muscle cells and hypertrophy is an enlargement of smooth muscle cells.
Diagnosis
Diagnosis requires a clinical judgement of patient history, physical examinations of symptoms, and pulmonary function tests. Pulmonary function tests include spirometry and peak flow rates to measure the airflow limitation. Typically, individuals have an early onset of asthma, but can occur at any age.
Spirometry measures forced vital capacity (FVC) and forced expiratory volume in the first second of expiration (FEV1) after maximal inspiration.
- Ratio =
- A decreased ratio indicates airflow limitation caused by airway obstruction
Peak flow is how fast an individual can blow air out of their lungs.
- Normal peak flow rates are determined based on height, age, sex, and race
- Adult peak flow rates range between 400 – 700 litres per minute
- Higher peak flow rates for men than women
- Low peak flow rates indicate asthma
Asthma Exacerbation
Asthma exacerbation, also known as an asthma attack, occurs when the severity of the disease or symptoms acutely worsen.
Prevention Before Exacerbation
- Trigger avoidance of stimuli such as allergens, pollen, smoke, chlorine gas or cold dry air
- Medications administered before exacerbations
- Inhaled corticosteroid orally
- Works slow
- Inhaled long-acting β2-adrenergic agonist
- Works to relax smooth muscle cells in the walls of airways to relieve the bronchoconstriction
- Both can be used in combination
- Inhaled corticosteroid orally
Treatment After Exacerbations (Rescue Therapy)
- Medications administered after exacerbations
- Inhaled short-acting β2-adrenergic agonists or bronchodilators
- Works quickly to decrease airway resistance
After the use of bronchodilator drug inhalation, there should be a substantial reversibility of airway obstruction (≥12% increase in FEV1).
Treatment for Allergy-Induced Asthma
Typically, during allergy season, the immune system recognizes substances such as pollen as foreign material to the body. The body will release chemicals to try and kill the substance. In addition to inhaled corticosteroid treatments, there is an injectable medication called Xolair. Xolair medication lowers IgE levels, which may help during allergy season by preventing immune and asthmatic responses.
Asthma Attack Symptoms
There are many triggers of an asthma attack. Some triggers are also allergy-causing substances and include things like mold, pollen, dust, and animal hair. There are many tests that can detect asthma are Arterial Blood Gas, Peak Flow Measurements, Pulmonary Function Tests and blood tests to measure eosinophil count.
Indications can happen every time the aviation routes are aggravated. Now and then indications are gentle and go away on their own particular or after negligible treatment with an asthma solution. Different times, indications proceed to deteriorate. At the point when indications get more serious and/or extra indications happen, this is an asthma attack.
What Do You Do During an Asthma Attack?
Common Symptoms of an Asthma Attack
- Coughing
- Chest pain or tightness
- Shortness of or gasping for breath
- Wheezing
- Flushed, pale, ashen or bluish looking skin
- Speaking in clipped or short bursts of speech
- Have the person STOP whatever activity he/she is doing.
- Send another person to get help. DO NOT leave the person alone.
- Follow the person’s Asthma Action Plan or emergency plan if there is one.
- If the individual has a QUICK-RELIEF INHALER or NEBULIZER (with medicines such as albuterol, proventil, ventolin, proair, relion, or xopenex), have him/her USE IT IMMEDIATELY!
Generally, during an asthma attack an individual should:
Prepare inhaler for use by shaking canister for several seconds. The person should exhale or empty all air out of lungs, and follow as listed below with or without a spacer:
- Inhaler With a Spacer or Holding Chamber:
- Place spacer with inhaler in mouth (lips and teeth around opening) Inhale 1 puff of medication by depressing the canister once, breathe in slowly and deeply, hold breath for 10 seconds and then exhale.
- Without a Spacer or Holding Chamber:
- Wait 30 seconds to 1 minute between puffs of inhaled medication.
- Place inhaler at the opening of the lips or a distance of 1 inch from open mouth; depress canister 1 time and inhale medicine quickly and deeply at the same time; hold breath for 10 seconds and then exhale.
- Shake medication canister for several seconds between puffs.
- Repeat process, depress canister and inhale another puff, hold breath for 10 seconds and exhale.
- Continue as needed, typically 4 to 8 puffs (depending on severity of symptoms and what is outlined in your Asthma Action Plan).
- Give sips of room temperature water.
- Have the individual sit up and slowly breathe in through the nose and out through pursed lips (pursed lip breathing). Pursed lip breathing technique is:
- Start by sitting comfortably in a chair. Do not lie down.
- Relax your shoulders and neck. Concentrate on not gasping for air as you drop your shoulders.
- Breathe in slowly through your nose. Concentrate.
- Purse your lips together tightly as if trying to whistle, and blow out slowly through your mouth. Take as much time as possible to exhale in this way.
- Relax. Keep using the pursed-lip breathing until the breathless feeling goes away. Rest between breaths if you feel dizzy
For More Asthma Information Read Here

